Last Wednesday, our day at Irvine Plastic Surgery Center started out at 8:00 A.M. with a patient who underwent removal and replacement of older silicone gel breast implants, and a lift. She also had just a little bit of liposuction of her hips. I knew she would do well. She had undergone a secondary tummy tuck at Hoag Hospital over this past Winter, and her post-operative course was splendid, unremarkable. Her original surgery on her breasts and abdomen had been performed about 11 years prior, by another surgeon.
The second patient on Wednesday underwent a partial tummy tuck removing just the ledge that hung over the C-section scar created at the time her twins were born several years ago. This patient opted not to have a full abdominoplasty, but rather the more conservative procedure, along with liposuction of her lower abdomen, hips, and flanks. She also did very well. The second surgery was completed about 3 P.M and the patient was driven home by her mother, uneventfully about 4 P.M.
The rule of thumb in my practice, is that patients who undergo ambulatory surgery remain locally the night after surgery, or at least within 30 minutes of the office. This is requested so that I have the option to see them during the first 24 hours after surgery. Frequently, my patients stay at the Candlewood Suites, Irvine, which is across from my office and the Hoag Hospital Irvine Emergency Room. The proximity allows the patient to be seen the evening of surgery, and first thing the next morning. Often, we wrap the hotel fee into our bundled pricing.
Typically, patients residing or having somewhere to recover closer than 30 minutes, go home with a family member. All surgical patients are required to have a responsible adult with them for 24 hours. My anesthesiologist reminds us that this is an order not a suggestion.
About 6 P.M. last Wednesday, I had just got home from work and was sitting down to dinner with my wife. I received a text with a photo from the mother and a friend of patient number 2 that the support garment placed on her surgical sites was soaked with blood tinged fluid. She also reported that she might have been a little light headed when she got up quickly.
What should I do?
I explained to the patient that the liposuction technique, known as tumescent liposuction, infuses a large volume of fluid and anesthetic into the tissue, to reduce discomfort and bleeding. Most of this fluid drains out on the garments, clothing, and bedding, over the first 12 to 24 hours and then it stops. Unless, otherwise prepared for this appearance, it can be alarming. I told her she was safe. She seemed reassured but was still faced with having to manage a dressing and perhaps an outfit change.
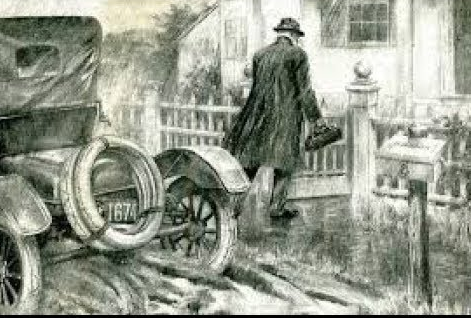
I knew she was okay. I waited a few minutes, and texted back “It may take a bit of time, but I will run by my office and get some fresh dressings, and a couple of new abdominal binders, and I will head over for a house call. According to my GPS, this would take about 45 minutes,” I said.
If it is a visit that I haven’t planned, I usually wait a few minutes before I make the decision to go, and then after having a short argument with myself, I head out.
The patient, her mother, and her friend seemed pleased and relieved to learn that I would be making a house call. They texted me while I was in route and asked if they could pick up a carry out meal for me. “Thanks, but no thanks,” I responded.
I have made hundreds of house calls on my surgical patients since going into practice many years ago. The visits always seem like the right thing to do. Once is a blue moon does the house call result in anything other than a well visit, a “reassurogram.”
As a result of the house call, the patients are re-assured that they are doing well, and I have had an opportunity to see how they are managing. An interesting strategic byproduct of the visit always occurs. The level of trust in the professional doctor-patient relationship is amped up exponentially. Patients remember the house call forever.
Whether it is at the local hotel, or half way across town, it is nice to check the surgical patient the evening after surgery. Maybe it is a throwback to the days of surgical residency when young doctors would round with their attendings on inpatient hospital patients every evening after work and early the next morning.
Over the years, I have found that using technology such as FaceTime, has allowed me to observe a patient’s status with an ability and confidence that prior hadn’t existed. Nevertheless, there is something about greeting that individual in person that seems as valuable as it must have been 100 years ago.
Last Wednesday night’s house call was a little different than any I had experienced prior.
After fighting traffic, and tolls, having my phone die, and losing my GPS signal, I finally found my patient’s home. I knocked on the door, and was greeted by a happy patient, her girlfriend, and her mother. After we able to determine all was good, and replace her surgical dressing with a fresh garment, there was a knock on the back door, on the kitchen door which opened into the common area of the condominium complex.
It was neighbor stopping by to say hello. In through the door walked a woman in her late 30’s who had been my patient, and a recipient of my signature house call many years ago. “Dr. Altman! nice to see you,” she said as she walked into the kitchen. I was surprised, pleased and greeted with a big hug – “one of my favorite patients!” I responded.
When I think back over nearly thirty years of practicing plastic surgery, I will always remember the house calls as part of the process that has been very meaningful to me – the chance to offer “peace of mind.” The visit lets my patients know that I care and that I am committed to their well-being throughout the course of their healing.
I have been offered dinner, pastries, pizza, coffee, and once in a terrible rain storm in Dana Point, a place to stay – all gestures of kindness by grateful patients. Typically, my response is “no thank you,” and I am on my way within 5 or 10 minutes.
There have been exceptions however. A few weeks ago, on a Saturday morning, I visited a patient that had undergone surgery several days earlier and was too sore to ambulate to the office. Her husband and son had made a special trip to buy hot glazed doughnuts and I couldn’t turn down such an offer.
I got home about 8:30 P.M. last Wednesday night and started to think about all the good things that had happened that day. I would still have to write notes on the two surgical patients of the day and prepare for the two new patients who would undergo surgical procedures the following morning.
I wonder where they live?
Donald Altman, M.D.
